|
AGENCY OVERVIEW REPORT
The Agency Overview dashboard report shows patient census, visit
statistics, episode and period breakouts for a 12 month or 12 day period.
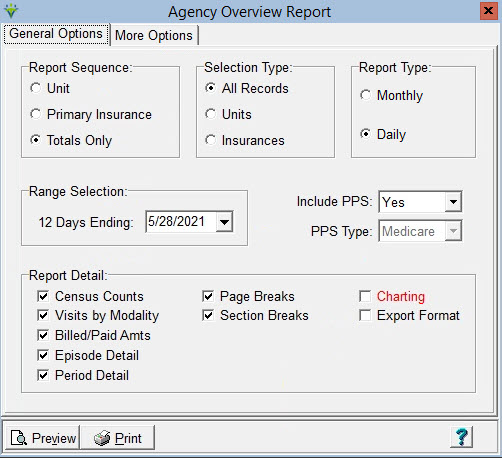
General Options Tab
Report Sequence: Determines how the report will
be sorted. Can choose Unit, Primary (Seq 1) Insurance or Totals Only.
Selection Type:
Choose all records or specific Units or Insurances
Report Type:
Choose Monthly or Daily Include PPS: Select 'Yes' for all records, 'No' to only include non-PPS records, or 'Only' to exclude non-PPS records. PPS Type: Enabled when 'Only' is selected for Include PPS option. Choose 'Medicare' or 'NY Caid'. Report Detail: additional drill-down options for each selection are available on the More Options tab. Census Counts: When checked, shows a beginning census, number of new admissions, readmissions, discharges, calculated ending census and Average Length of Stay by month or day. Page Breaks: When checked, the report will start on a new page based on the Report Sequence selected (i.e. by Unit or Primary Insurance). Visits by Modality: When checked, shows billed visit counts by modality. If Billed/Paid Amts also checked, these amounts are included in the Visits by Modalty section. Export Format: Select to create a XLS file that can be opened in Excel. Billed/Paid Amts: Select
to show Billed and Paid Amts in the period. Shows in Visits by Modality
section if that option is checked, or in the Census Count section if
Visits by Modality is unchecked. Use Process-Date: Enabled when Billed/Paid Amts is checked. If selected, the Billed/Paid amounts are included based on Process date (i.e. the date a billing audit or payments/adjustments were posted) vs. showing based on the Bill Date or Paid Date entered. Episode Detail: When checked, shows certification and recertification counts along with average case mix weights, average EEP, LUPA and Therapy Upgrade/Downgrade episode counts. Period Detail: Enabled when Include PPS has 'Yes' or 'Only' selected'. When checked, shows counts for Period 1 and Period 2 PDGM billing as well as the average case mix weight, average EEP, and LUPA counts for each. Only RAP Billed: Enabled when Include PPS has 'Yes' or 'Only' selected'. When checked, will only count periods that have had a RAP Billing Audit posted for the Period Detail reporting section. Only Final Billed: Enabled when Include PPS has 'Yes' or 'Only' selected'. When checked, will only count periods that have had a Final Billing Audit posted for the Period Detail reporting section. Charting: Check this box for a Bar Chart view of the information (example report below). Export Format: Check this box to export the report to Excel format. Press Print, then save as a.xls. More Options TabCheck or uncheck the box to select the level of detail to be shown on the preview or charting report. 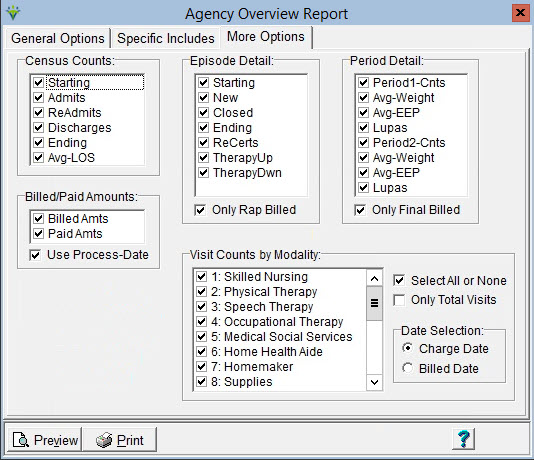 Sample Charting: 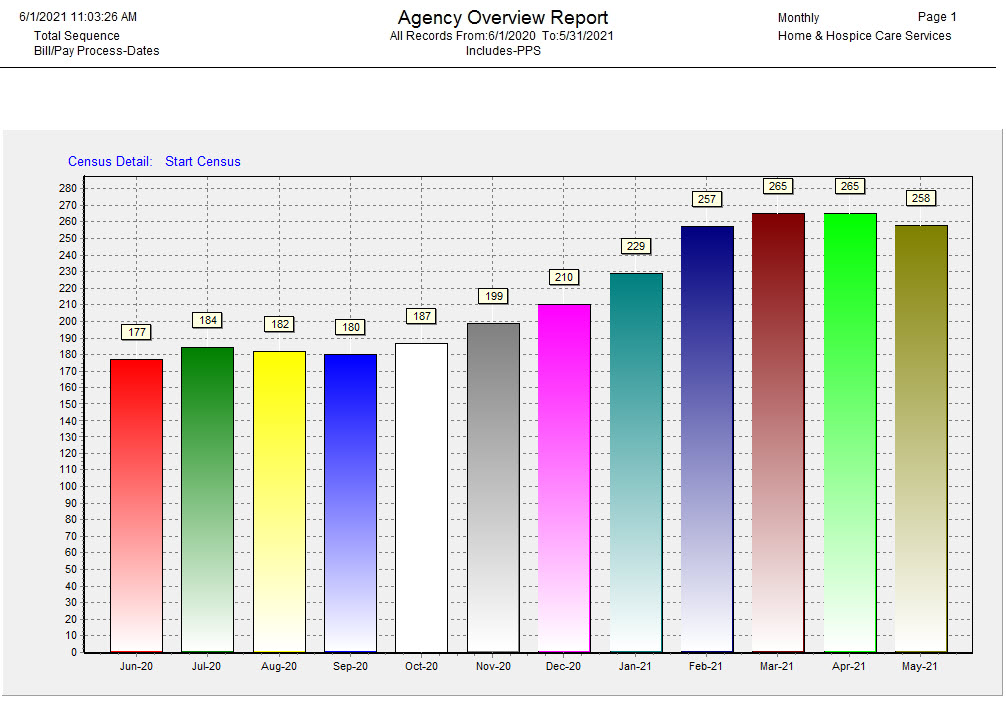 Sample Report: 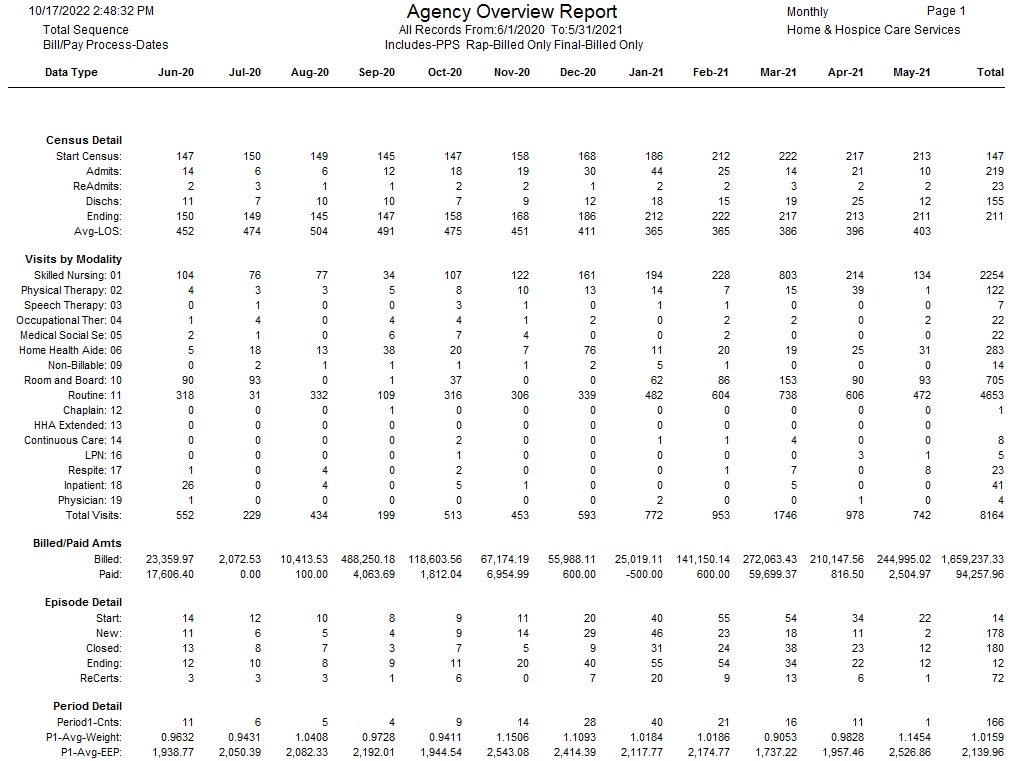
Report Explanation: Report columns are broken
out by the 12 months or days preceding the user-specified Ending Date,
depending on the report type chosen. Admits: Number of patients admitted in the period
(including readmits). Readmits: Number of patients readmitted in the period. Dischs: Number of patients discharged in the period. Ending Census: This is the Starting Census + Admits – Discharges. The ending census becomes the starting census for the next month. Avg-LOS: Average Length of Stay days in the period for active patients. *The Total column takes
the starting census from the beginning of the reporting period and adds the
total admits and discharges for the reporting period to get the ending census. Visits: Number
of visits in the period based on charge date (must be billed).
Can be tied back to visit counts on the Statistical Analysis report for Billed visits. Billed: Dollars billed in
the period based on A/R Bill Date. Inclusive of RAP and Final billed amounts for PPS and PDGM payers. Can
be tied to A/R billed amount on the Accounts Receivable report. Paid: Payments applied in the period based on
payment date. Can be tied to the Payment
Report. Episode Detail Start Episodes: Number of open
episodes at the beginning of the reporting period. New: Number of episodes starting in the reporting period based on episode start date. Closed: Number of episodes ending during the reporting period based on patient’s discharge date or episode end date. Ending Episodes: This is the number of Starting Episodes + New – Closed episodes. Recerts: Number of the recert episodes. Therapy-Ups: Number of closed episodes that have a Therapy Upgrade. Therpay-Dwns: Number of closed episodes that have a Therapy Downgrade. Period Detail Period1-Cnts: Number for Period 1s included for that month/date Period2-Cnts: Number of Period 2s included for that month/date Avg-Weight: Average case mix weight for periods included in date range. Note: this number may not match PPS Revenue Report or PPS Margin Report due to no consideration of billed status. These figures are broken out for Period 1 and Period 2. Avg-EEP: Average case EEP for periods included in date range. Note: this number may not match PPS Revenue Report or PPS Margin Report due to no consideration of billed status. These figures are broken out separately for Period 1 and Period 2. LUPAs: Number of the closed periods that are LUPAs. These figures are broken out separately for Period 1 and Period 2.
|