|
Authorization Report The Authorization Report provides a way to track the number of visits, hours or units used against what the insurance has authorized for patients. The agency can then determine which payers need to be contacted to obtain additional authorizations for patients as needed.
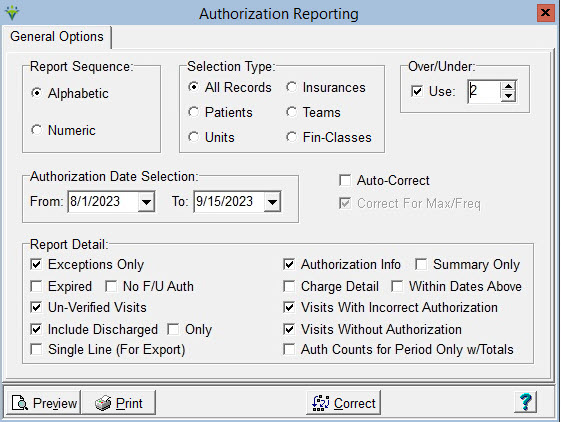
Report Sequence: Select Alphabetic or Numeric Selection Type: Specify All Records or Specific Patients/Units/Insurances/Teams/Financial Classes via the 'Specific Includes' tab. Over/Under: check the Use box and specify the number of visits remaining before the patient will have met their authorization limit. This allows the user to select how many visits are remaining before they need to contact the payer to obtain additional authorizations. Patients who have exceeded their authorization limit will also be included.(Exceptions Only must be checked). Authorization Date Selection: Enter From and To Dates for the authorization date range. The report will show authorization records active within the date range specified. Auto-Correct: Check this box to attach an authorization number to charges if there is a match on the Care Type and if the authorization dates cover the charge date. Charges will be attached to the authorization number even if they are over the maximum authorization limit and even if they exceed the authorization frequency (to disallow this, check the box for 'Correct For Max/Freq; see below). If charges exceed an authorized max/frequency and a subsequent auth is found for the date and Care Type of the charge, they will be attached to the subsequent authorization number. The Auto-Correct option should be run when an authorization is added or changed after the visit was entered or scheduled. Correct for Max/Freq: Check this box to detach charges from an authorization number if they have exceeded the authorization maximum or if they are over the authorized frequency. The 'Auto-Correct' option must also be checked when running this. Report Detail: Select which Authorization information to print on the report Exceptions Only: Shows authorizations that are over or under the max amount and the charge detail will identify charges that fall outside the frequency limits. Expired Only: Only prints Authorizations that have ended within the From/To date range selected. No F/U Auth: Same as 'Expired Only' option but excludes expired auths that have a follow up authorization with the same Care Type or charge code. Un-Verified Visits: Includes scheduled visits that have not yet been marked completed/verified. Include Discharged: Includes Authorizations for Discharged Patients. 'Only': check this box to show auths for only discharged patients. Active patients will not be included. SIngle Line (For Export): Check this box to print the report to an Excel file instead of to PDF. Authorization Info: Select to print authorization detail. The authorization Start/End dates, Authorized By and Authorization Number will show on the report. Summary Only: When checked, does not show authorization detail on the report and instead shows only total amounts for the admit. Charge Detail: Select to print visit detail information on the report Within
Dates Above: Check this box to only see charges that occur within the Date
Selection specified. Un-check this box to include all charges within the
authorization period. Visits with Incorrect Authorization: This is a legacy option that would only be needed to show visits attached to an authorization that was later changed to a different Care Type or effective dates. Visits Without Authorization: Select to print visits not attached to any authorization. Auth Counts for Period Only w/Totals: Select to print actual and authorized visits and dollar amounts based on the From/To report date range. Sample Report: 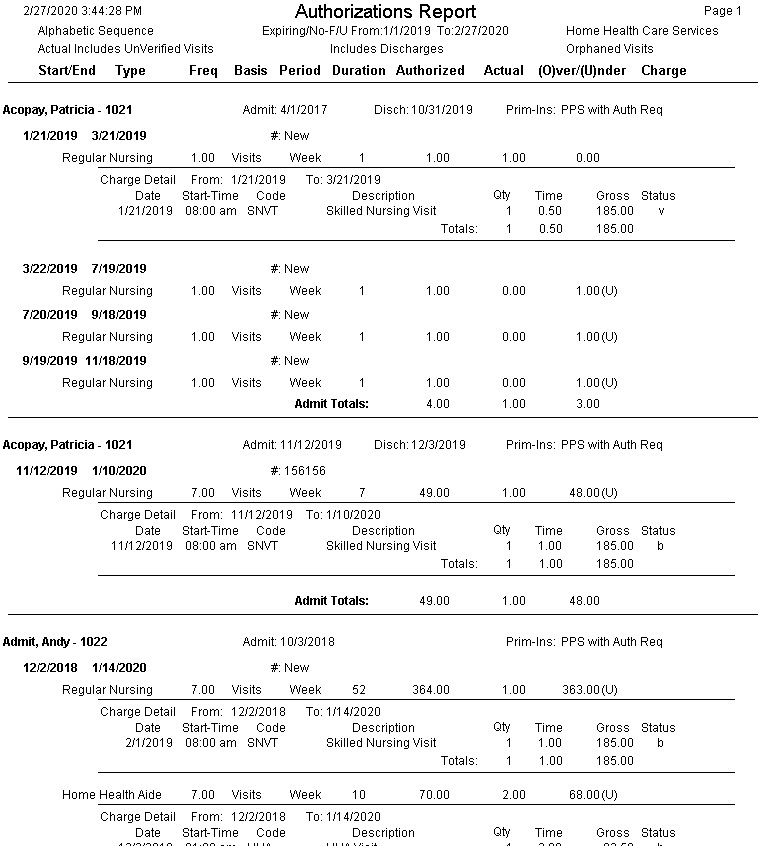
|
| Status Legend: v = Verified b = Billed |