|
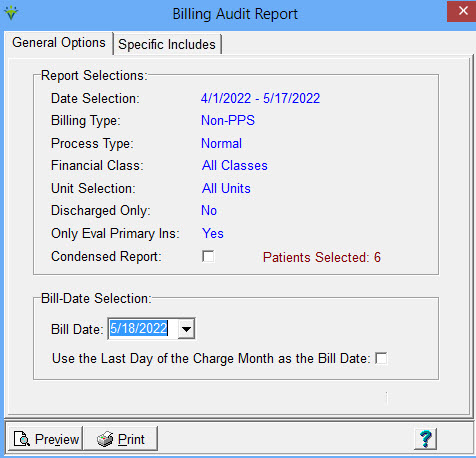
Billing Audit
The Billing Audit is run from the Billing > Pre-Audit or Charge
> Hospice LOC Report. After running either report for "Ready to
Bill" and closing the preview window, a Bill Audit button will
appear. It provides the
ability to review patient insurance information and rates for
accuracy prior to printing bills or creating electronic claims. Report
Selections are copied forward from selections made on the Pre-Audit or
Hospice LOC Report.
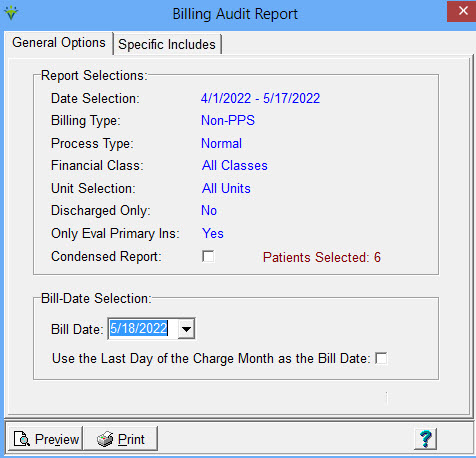
Date Selection: Displays the From and To Dates specified on the Pre-Audit or Hospice LOC Report. For
Normal
audits, this applies to charge dates within the date range. For
PPS Final audits, this applies to periods that end in the date range.
For PPS RAPs, this applies to periods starting in the date range.
Billing Type: Non-PPS and Hospice indicates per-visit payers. PPS indicates the run is for PPS periods.
Process Type: Medicare
Final (for Medicare & MA payers), Normal (Fee-for-Service
payers), NY Caid RAP (NY Medicaid EPS payers), or NY Caid
Final.
Financial
Class: displays the Financial Class if specified on the Financial Class
drop-down of the Pre-Audit or Hospice LOC Report. Displays
"Selected Classes" if the Selection Type is set to Fin-Class. Displays
"All Classes" if no Financial Class selection was made. Unit Selection: displays the Unit specified on the Unit drop-down of
the Pre-Audit or Hospice LOC Report. Displays "Selected Units" if the
Selection Type is set to Unit. Displays "All Units" if no
Unit selection was made. Discharged Only: This option copies over from the user
selection made on the Pre-Audit or Hospice LOC report. If checked, only
audits discharged patients will pull. Active patients will
not be included in the run. Only
Eval Primary Ins: This option copies over from the user selection made
on the Pre-Audit or Hospice LOC (More Options tab) reports for
"Only Evaluate Primary Insurance." Condensed Report: if checked, the audit will not page break by patient and information will be summarized. Patients Selected: displays the number of patients listed on the Specific Includes tab.
Bill Date Selection: Enter the date to be used as the A/R aging
date (for
Normal
and PPS RAP Process types). A/R reports and claim generation require
entering the bill date as selection criteria.
Use Last Day of Charge Month as Bill Date: Check this box if using a
Charge Date selection that spans multiple months and you want to
create separate A/R records for each charge month. The last day of
the charge month will be assigned as the Billing Date. Available for ‘Normal’
process type. Only appears if "Close Day of Month" is not set in System Settings. (Optional). Retroactive
Billing: This option only appears if "Close Day of Month" is set in
System Settings. Only Bill Dates within the closing date range can be
used unless this box is checked. For RAPs, only today's date or a
future date may be used. If checked, the user must choose an existing
Bill Date for posting (for example, posting late charges to be
billed on existing claim or if the original claim has been un-billed.)
Press Post to post
the Billing Audit after it has been reviewed for accuracy. Once posted,
a Billing Audit cannot be re-printed unless an Un-Bill is done first
under the Payment Entry>Detail screen.
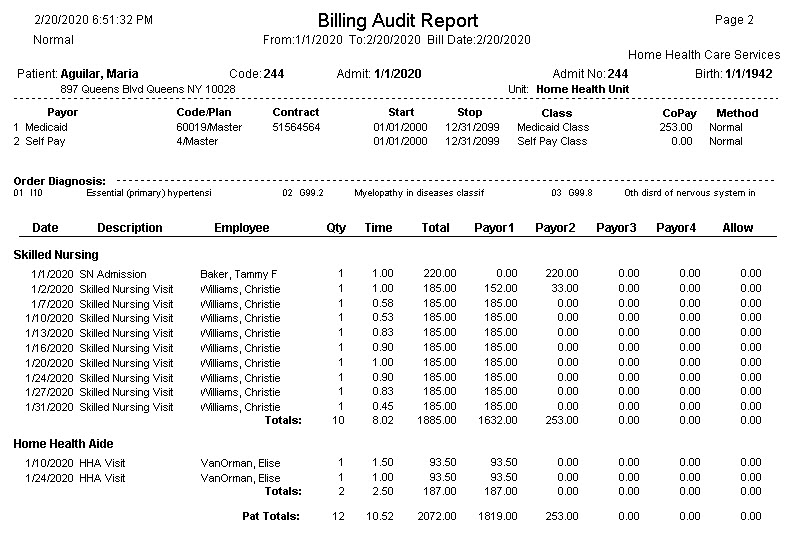
Sample Normal Audit with CoPay: 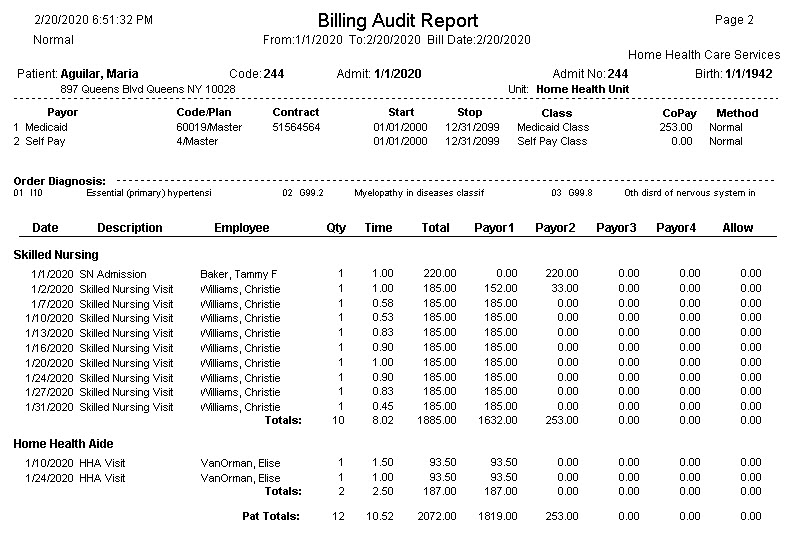
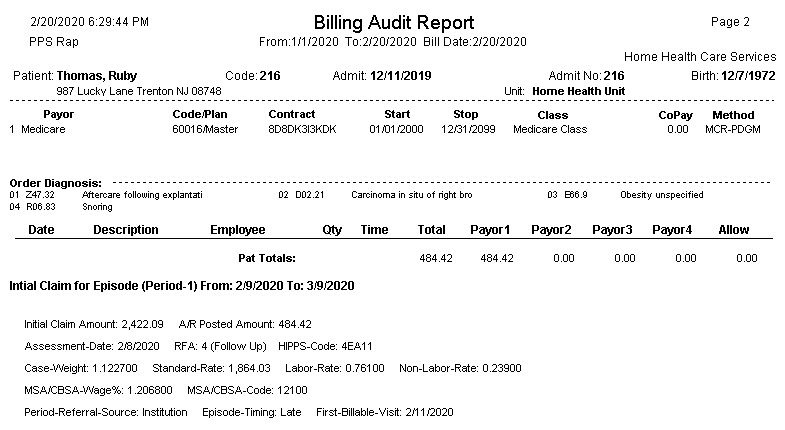
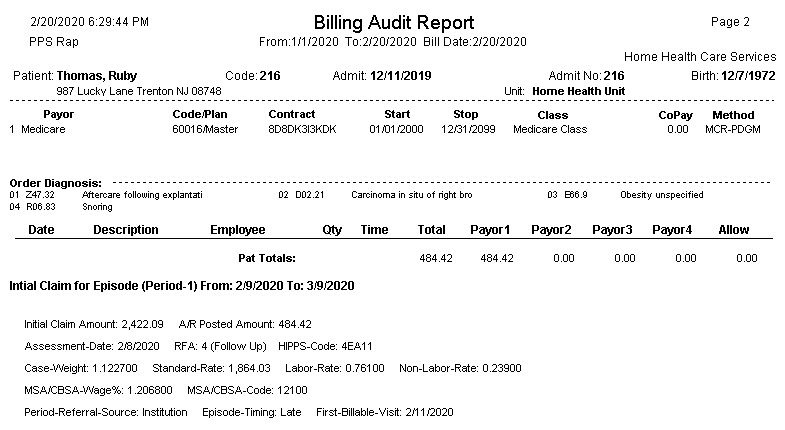
Sample Medicare PDGM RAP Billing Audit Report:
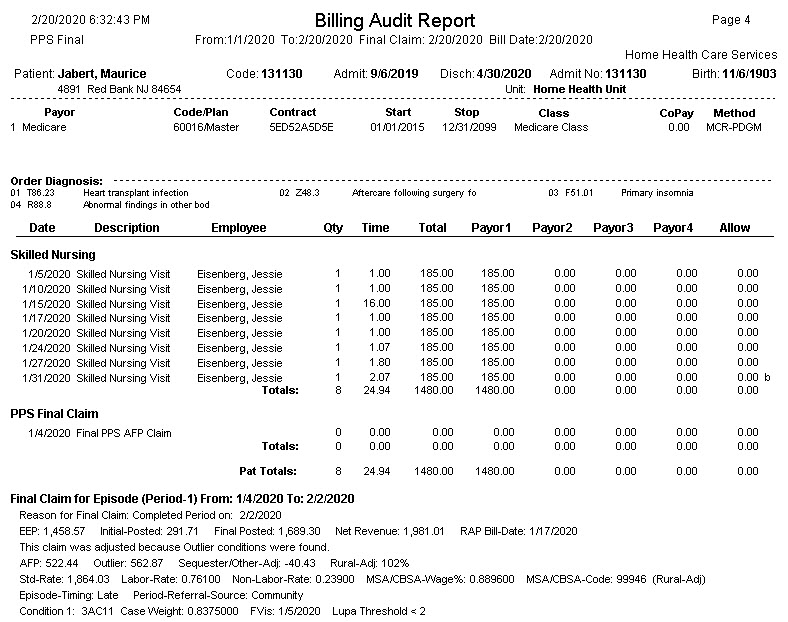
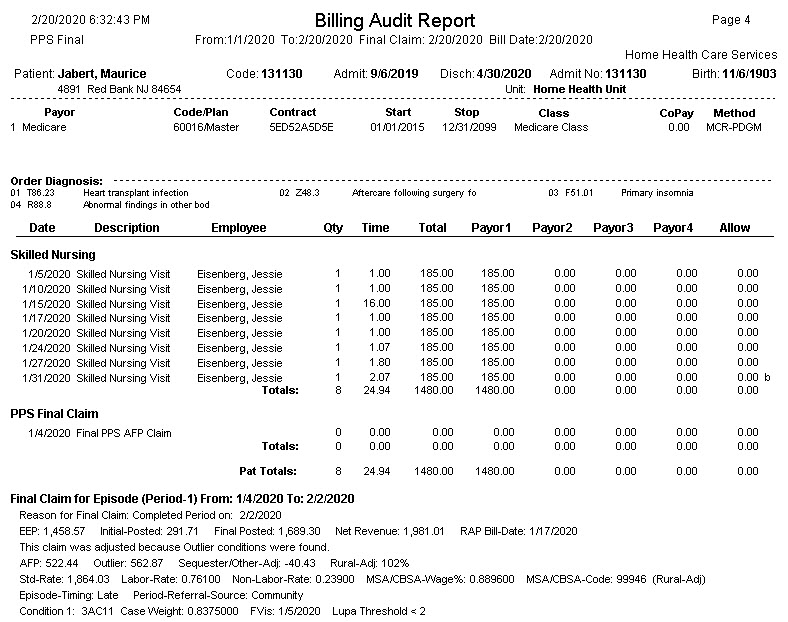
Medicare PDGM Final Billing Audit Report:
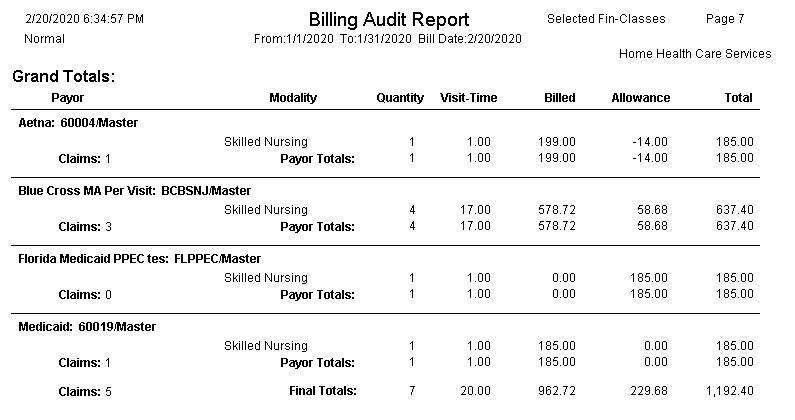
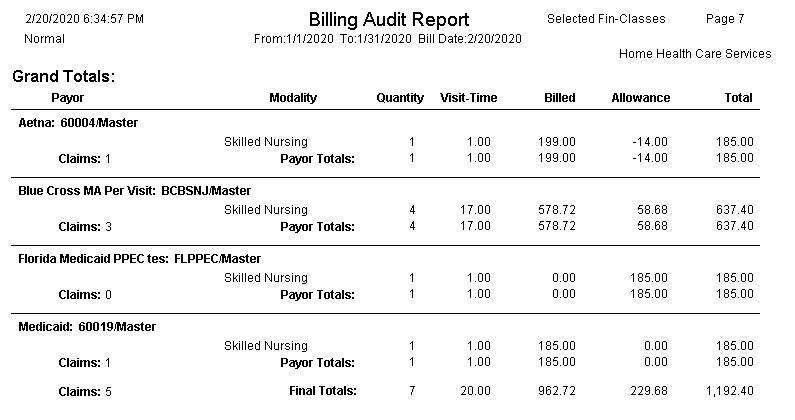
Sample Insurance Totals Page:
|