|
DENIAL REPORTING Denial Reporting provides the ability to view which claims that have been marked "Deny" in the A/R > Payment/Transfers menu via the Detail tab due to an insurance claim denial. In addition to manually entered denial information, claim adjustment reason codes for Line-item zero dollar payments posted posted electronically will be included on this report if the the charges were billed with Line Item Control Numbers (REF*6R segments).
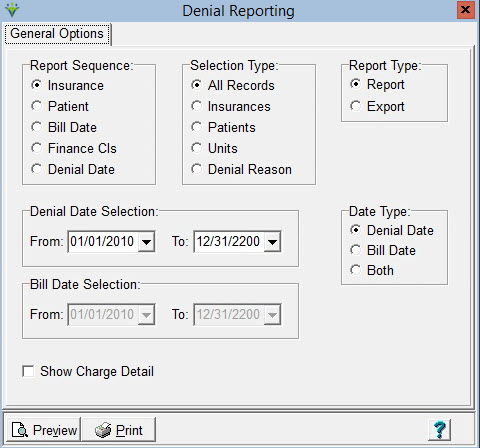
Report Sequence: Set to print the report by Insurance, Patient, Bill Date, Financial Class, or Denial Date Selection Type: Select to print report for All Records, or for specific Insurances/Patients/Units/Denial Reason Report
Type: Select Report or Export (creates an XLS file). The most
recent DCN for the Payment record with the denial will pull to the
Export file but will not display on the Report. Denial Date Selection: Select Date Range (based on the Date Type selected) Date Type: Select to use either the Denial Date, Bill Date, or both as Date Selection criteria for the report Show Charge Detail: Check to display visit detail information on the Denial Report.
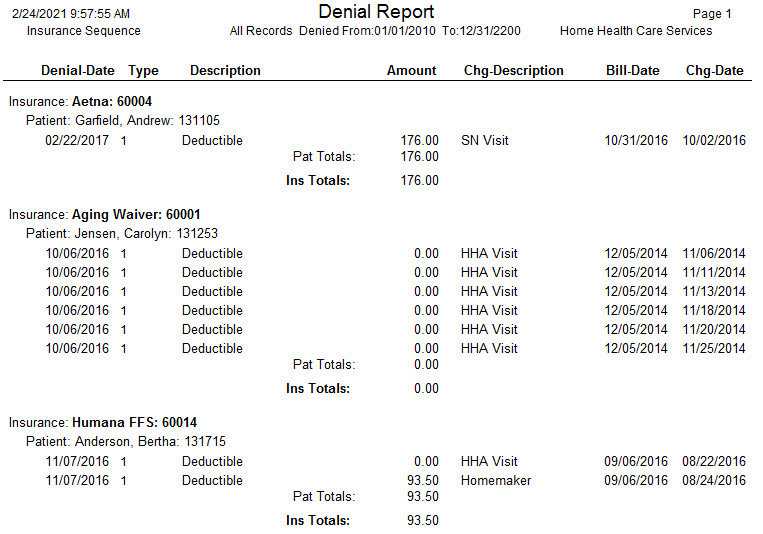
Sample Report:
|