|
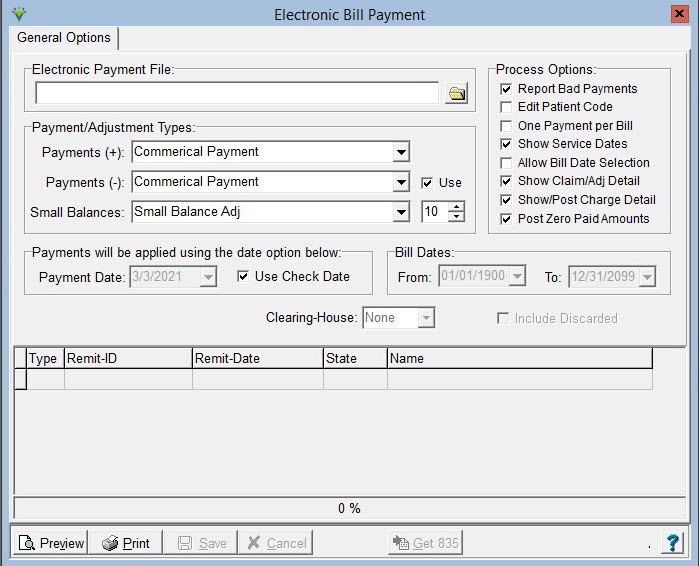
ELECTRONIC BILL PAYMENT Electronic Payments provides the ability to view and post
electronic remittance advice (ERA) files to the system.
Electronic Payment File: Browse to locate the 835 file that was
downloaded from your payer’s site. Process Options: Report Bad Payments: If checked, the report will display payments that will NOT be posted. Bad Payments may occur if processing a remit file that includes payments for claims that were not generated out of HBS. Edit Patient Code: Used if applying one ERA file across multiple datasets. If checked, the system will look for a match on the Patient Code as well as Patient ID and Bill Master ID prior to posting. One Payment per Bill: If checked, multiple payments per bill record will be summarized into one net payment line. Used primarily for NY Medicaid remittances. Show Service Dates: if checked, individual charges will show on the report output. Allow Bill Date Selection: if checked, the Bill Date From and To selections are made available and the remittance can be posted only for bill records within the selected bill date range. Show Claim/Adj Detail: if checked, the report will show the adjustment code and amount at the claim level as well as the charge level. Show/Post Charge Detail: if checked, payments received at the charge level will be posted to the charge detail level. If unchecked, the summarized payment amount will be posted at the claim level instead. (NOTE: in order to post remits at the charge level, claims must be submitted to the payer with the Loop 2400 REF*6R segment set to pull the 'Line Item Control Number'). Post Zero Paid Amounts: check to post zero dollar payments. Payment
(+) and Payment (-) Types: Choose the payment code(s) to use
when posting positive and negative amounts. If the Payments (-)
'Use' option is not selected the same payment code will be used
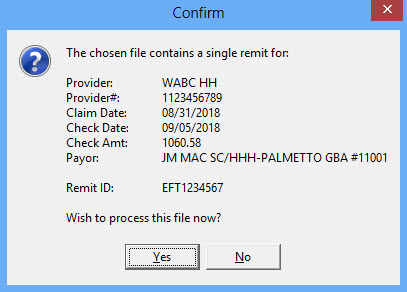
for all payments. Small Balances: Optional. Choose a payment code to use and enter a dollar amount (max is $10 and will adjust both credits and debits) to use for posting an additional payment to zero out the A/R after the insurance payment has been applied. Bill Dates: Optional. Choose a date range for the bill master records that payments will be posted to. Payment Date: Defaults to Today's Date. Can be changed to a different date, or can select "Use Check Date" as the payment posting date. Clearing-House: If contracted for a Clearinghouse interface, choose that interface from the drop-down to enable the "Get 835" button. Refer to the Ability Interface Reference Guide for information on the Ability Interface or the Zirmed Interface Reference Guide.When the Preview is selected, select Yes to process the file:
ERA files cannot be double-posted. If a user tries to post a payment file that has already been posted, the report will show that $0 will be posted. Sample Report: 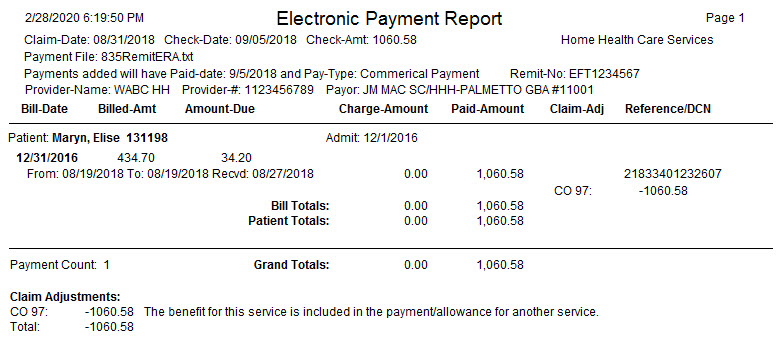 |