|
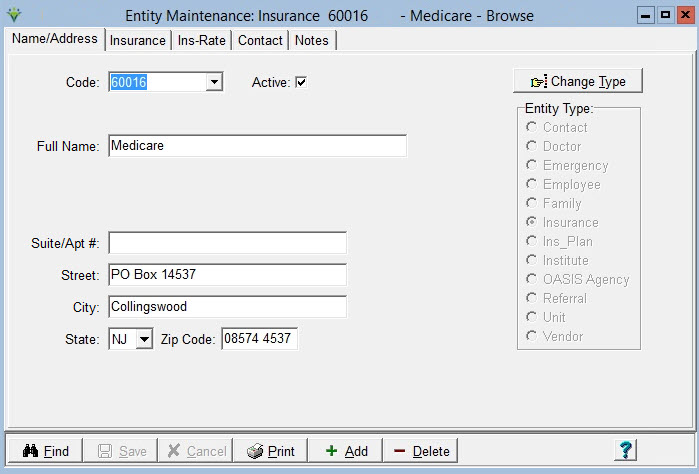
Insurance Insurances are entered for patients in the Clinical Patient Profile and can be viewed in the Billing Module in the Patient file Insurance tab. A new insurance should be stored to the appropriate electronic claim option set prior to creating claims. Go to File > File Maintenance > Entity press Change Type and set the radio button to Insurance.
To Update/Maintain Insurance Information: Go to the Clinical Insurance Library to enter or update the name and address information.Insurance tab
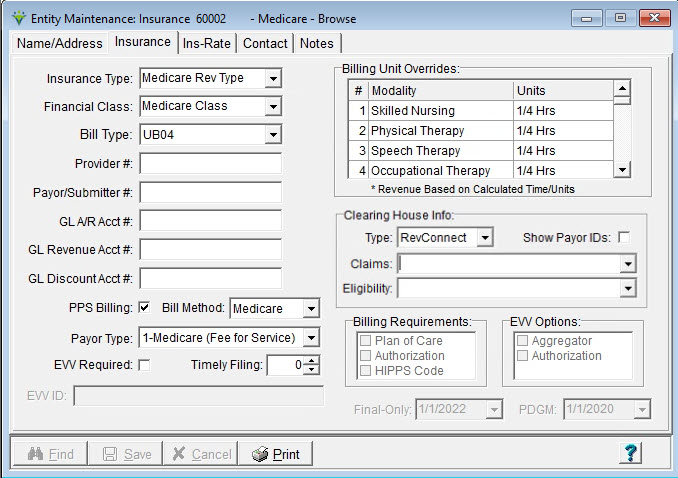
Insurance Type: payers are grouped by type if they use the same Revenue/HCPCS/Modifiers on claim output. Select from the drop-down (Insurance Types are created in File > File Maintenance > Category). For example, if the insurance uses the same codes revenue & HCPCS as Medicare, select the Medicare Rev Type here. When assigning revenue/HCPCS/modifiers to charge codes, they are added based on Insurance Type. Financial Class: (Insurance Class) groups payers for purposes of running the billing process, claim generation and reports. (Classes are created in File > File Maintenance > Category, Insurance Class Type). Bill Type: Select the claim format to be used for claim generation. This setting can be bypassed at the claim level if 'Any Form Type' is checked. The payer designates which form type they accept. Provider #: Enter the provider number assigned to your agency by the insurance company. Optional. Payer/Submitter #: Enter the 5-digit electronic claim payer ID assigned to the insurance based on the Clearinghouse or claim receiver designation. GL Revenue Account #: Enter the Revenue account number for your agency's General Ledger. Obtain this number from your Accounting department. GL Discount Account #: Enter the Allowance account number for your agency's General Ledger. Obtain this number from your Accounting department. PPS Billing: check this box if the payer reimburses based on Medicare PDGM billing rules. Bill Method: For Medicare Home Health and Medicare Advantage payers who reimburse the same as Medicare, set to 'Medicare.' For Medicare Hospice and payers who reimburse the same as Medicare, set to 'Hospice.' For NY Medicaid EPS, set to 'NY Caid.' Otherwise set to 'Normal.' Payor Type: Determines the value for element SBR09 Claim Filing indicator in electronic claim files. (i.e. MA for Medicare, MC for Medicaid and Title Programs, CI for Private Insurance and Unknown (Commercial), VA for Other Gov't, BL for Blue Cross.. Also used to determine if insurance is Medicare to allow for Real-Time Eligibility functions. EVV Required: check this box if using Netsmart Electronic Visit Verification
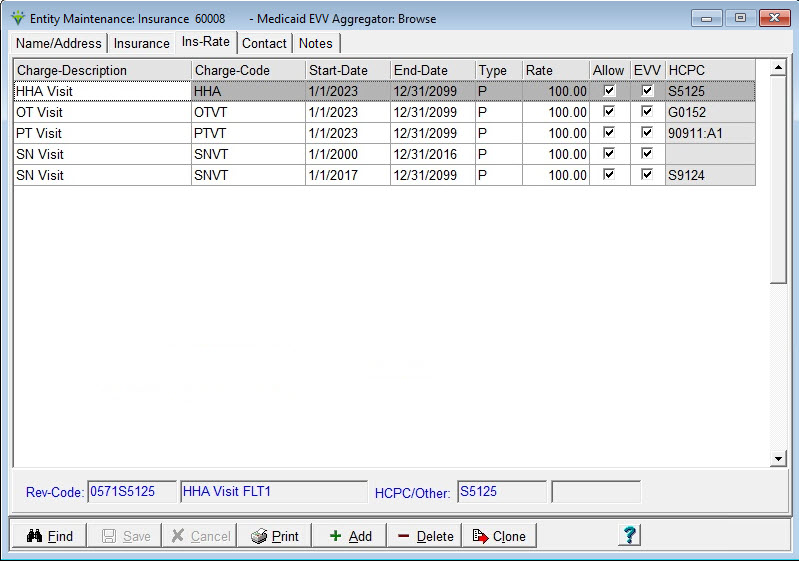
functionality for this payer. Only enabled if EVV is configured for the agency. EVV ID: setup for this item will be completed during EVV implementation. This information comes from the Clinical Insurane Library and is a combination of the Payer and Plan ID, seperated by a colon (ex: CRM2:732F5858-5C2B-4220-07E6-4D1825297702). Obtain these values from MCG+. Only enabled if EVV is configured for the agency. Billing Unit Overrides: overrides the Itemizations chosen in the billing Option Sets so multiple payers can share one Option Set even if their unit requirements are different. Modalities 1-40 are available for unit overrides. N/A This is the default option and means no payer override has been selected. The system will use Units set at the Option Set level instead. Units: Units on the claim is equal to visit quantity (e.g., 1 visit = 1 unit, regardless of visit time) Hours: Units on the claim is based on actual visit time (e.g. 1 minute visit = 1/60 = .02 units) *1/2 Hrs: Revenue and units will be based on visit time (rounded to 30 minutes) and uses the Insurance Rate (if present) or Charge Code Rate (see Colorado Medicaid FAQ). 1-44 minutes = 1 unit45-74 minutes = 2 units 75-104 minutes = 3 units 1/4 Hrs: Units on the cliam will be based on visit time rounded to the 15 minute increment. 1-22 minutes = 1 unit23-37 minutes = 2 units 38-52 minutes = 3 units 53-67 minutes = 4 units 68-82 minutes = 5 units 83-98 minutes = 6 units 1/2 Units: Units on the claim will be based on visit quantity multiplied by 2 (e.g. 1 visit = 2 units) 1/4 Units: Units on the claim will be based on visit quantity multiplied by 4 (e.g. 1 visit = 4 units) 1/x Units Units on the claim will be based on visit quantity multiplied by x (value of x can be entered in electronic Option Set locator 2390.22 or will default to 8 (e.g. 1 visit = 8 units) Charge Gross: Units on the claim will show visit quantity multipled by charge code gross amount (File > File Maintenance > Charge Codes, Bill Rate tab). *1/4 Hrs: Units on the claim will show visit time rounded to the 15 minute increment. Revenue will be based on visit time and will use the Insurance Rate if present or Charge Code rate. (see Indiana Medicaid FAQ). 1-22 minutes = 1 unit (revenue is 1/4 of the hourly rate)23-37 minutes = 2 units (revenue is 1/2 of the hourly rate) 38-52 minutes = 3 units (revenue is 3/4 of the hourly rate) 53-67 minutes = 4 units (revenue is equal to the hourly rate) 68-82 minutes = 5 units (revenue is 1 1/4 of the houlry rate) 83-98 minutes = 6 units (revenue is 1 1/2 of the hourly rate) *Hrs Rounded: Units will be based on visit time. Revenue will be based on visit time and use the Insurance rate if present or Charge Code rate. Note, time less than the first 30 minutes is still rounded to 1 unit but after that partial units of service 29 minutes or less round to the next lowest unit and 30 minutes or more rounds up to the next highest unit. If electronic claim Option Set locator 2390.12 is set to Revenue Code/Date Consolidation, time for the day will be totaled and then units calculated (see Indiana Medicaid FAQ or Colorado Medicaid FAQ). 1-89 minutes = 1 unit (revenue is 1 x hourly rate)90-149 minutes = 2 units (revenue is 2 x hourly rate) *Hrs Round Up: Units will be based on visit time. Time is calculated up to the next hour (see Colorado Medicaid FAQ). 1-60 minutes = 1 unit (revenue is 1 x hourly rate)61-120 minutes = 2 units (revenue is 2 x hourly rate) 121-180 minutes = 3 units (revenue is 3 x hourly rate) 181-240 minutes = 4 units (revenue is 4 x hourly rate) *OH Medicaid: Used for Ohio Medicaid billing (see OH Medicaid FAQ). 1-15 minutes = 1 unit (revenue is [1 x unit rate])16-34 minutes = 2 units (revenue is [2 x unit rate]) 35-45 minutes = 3 units (revenue is [Base rate]) 46-60 minutes = 4 units (revenue is [Base rate]) 61-75 minutes = 5 units (revenue is Base rate + [1 x unit rate]) 76-90 minutes = 6 units (revenue is Base rate + [2 x unit rate]) *FL PPEC: Used for FL Medicaid PPEC Nursing and CMS Therapy billing (see FL Medicaid and CMS Therpay Billing FAQ). Therapy:1-14 minutes = do not bill 15-29 minutes = 1 unit 30-44 minutes = 2 units 45-59 minutes = 3 units 60-74 minutes = 4 units 75-89 minutes = 5 units Nursing: 0-4.25 hours/day = Partial Day (code T1026) billed in hour units 0-59 minutes = do not bill 60-75 minutes = 1 unit 76-135 minutes = 2 units 136-195 minutes = 3 units 196-255 minutes = 4 units 4.26 - 12 hours/day = Full Day (code T1025) billed as 1 unit *LA PDHC: Used for LA Medicaid PDHC billing (see LA Medicaid PDHC Billing FAQ) Nursing: 0-6 hours/day = Partial Day (code T1026) billed in hour units 0-29 minutes = do not bill 30-89 minutes = 1 unit 90-149 minutes = 2 units 150-209 minutes = 3 units 210-269 minutes = 4 units 270-329 minutes = 5 units 330-360 minutes = 6 units 6.01 - 12 hours/day = Full Day (code T1025) billed as 1 unit Clearinghouse: Select Zirmed (Waystar), Ability, or RevConnect Type from the drop-down if contracted with Netsmart for one of these options. Show Payor IDs: check this to search for the 5 digit payer ID instead of payer name. Claims: select the 5 digit payer ID assigned by the clearinghouse for the payer for electronic claim submission. Eligibilty: select the RevConnect 5 digit payer ID for the payer for eligibility verification. Billing Requirements: These boxes are enabled when PPS Billing is un-checked. Checking any of the first three boxes will create a Failure message on the Billing Pre-Audit if the required information is missing. The Authorization flag is updated from the Clinical Insurance library. The VBP Adjust option should only be checked for payers applying VBP adjustments to PPS claims. EVV Options: Only enabled if EVV is required. Check the Aggregator box if Netsmart MCG+ is the Aggregator for the State Medicaid payer. Check the Authorization box if the State Medicaid program requires authorization information be sent to MCG+ as part of their EVV information requirements. Final-Only: shown only if PPS Billing is checked and can be changed if Payer Type is set to 2 - Medicare Advantage. Defaults to 1/1/2022 but can be changed to a valid date through 12/31/2024. PDGM: shown only if PPS Billing is checked and can be changed if Payer Type is set to 2 - Medicare Advantage. Defaults to 1/1/2020 and once enabled cannot be changed to an earlier date. Ins-Rate tab If your agency has contracted rates for this payer, enter them here to override the net rate setup at the charge code level. If the payer reimburses the same amount for charges based on Modality, add a Blanket Rate charge. If the payer doesn't cover specific charge codes, these should be added with a rate of 0.00. Revenue and HCPCS information for the charge code displays on the bottom of the window. If the incorrect codes are shown, refer to the Correcting Revenue & HCPCS FAQ . Refer to the Sequestration FAQ for instructions on maintaining the CMS sequestration rate.
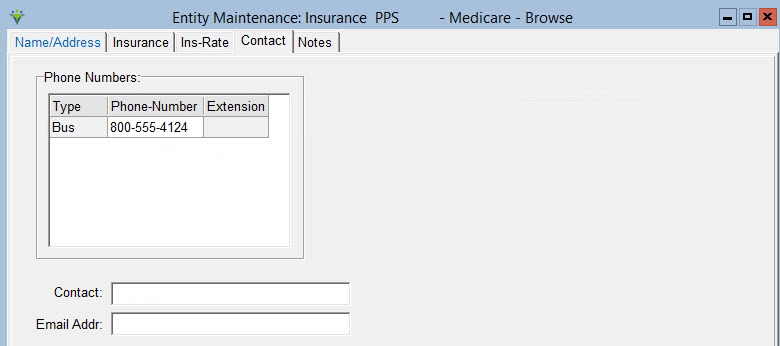
Press Add to add a new row. Charge-Description/Charge-Code: Select a charge description or code from the drop-down. Start-Date: Enter the effective date for the rate amount. End-Date: Enter the ending date for the rate amount or leave blank if unknown.. Type: Select 'F' if entering a flat dollar rate amount or 'P' if billing a percentage of the agency's Usual & Customary rate for the charge code. Rate: Enter the dollar or percentage amount for this charge (based on Type selected). Allow: If checked, when the billing audit is generated, any amount not covered by the payer will be written off to an Allowance account. If unchecked, the system will send the non covered dollars to the next active payer for the patient instead. If no additional payers are found, the non covered amount will be written of to an Allowance account. EVV: check this box for each visit that needs to be tracked by Electronic Visit Verification for this payer. Only displayed if EVV Required is checked on the Insurance tab. HCPC: view only field that displays the insurance HCPCS and modifiers for each service code. To change a HCPCS, go to File > File Maintenance > Charge Code. Active-Only: if checked only rates that are active for the current date will be shown. Un-check to view historical rates. Contact Tab Go to the Clinical Insurance library to add or change the business phone if needed. A fax number, email address and contact name can be added in the Billing Module if desired.Optional.
Notes tab Click Print to preview or print a complete Insurance List. |