|
Admit Stores patient referral, admit and discharge information. Data can be included on Patient Cover Sheet and/or Patient List reports. Click on PATIENT>ADMIT/MAINTAIN>Admit Tab
To Add a record on the Admit tab: Press
the Admit-Date: Enter the date the patient began receiving services from your agency. When adding a new admit record for a patient, the previous admit record must already have the discharge date and reason entered. Disch-Date: Enter patient's discharge date. Referral-Date: Enter Date the patient was referred to your agency. Defaults to today's date. Cover-Sht: Defaults to checked. Flags the patient for Cover Sheet printing when selecting to print Cover Sheets for "All Flagged Patients" under Patient>Cover Pages. You can also print individual Patient Cover Sheet by clicking "Print" button at the bottom of the Admit tab. Late: For Home Health patients, this gets checked if the Late option is selected in the Clinical Patient Profile or it's determined the patient is Late period based on prior discharge date. Used to calculate a Late HIPPS instead of Early for the initial billing period of this admission. For Hospice patients, this gets checked if the Hospice SOC Reason in the Clinical Patient Profile is set to a transfer or revocation reason. Used in the Hospice LOC Report to determine Early vs. Late Routine days. Adm-Src: Select the Admission Source from drop-down list. Defaults to "1 - Non-HCF (Doctor)". This information is used on claim output. Unit/Team tab
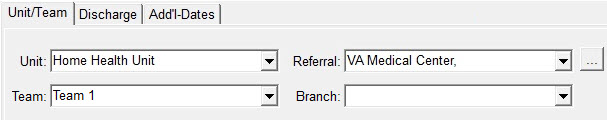
Unit: Select patient's unit as established under File>File Maintenance>Entity>Type = Unit. Required for Admitted patients. Referral: Enter the referral source. Add a new referral record by clicking on the "..." button or select from drop-down list. Optional. Team: Assign the patient to a Team. Teams are set up under File>File Maintenance>Category>Type = Team Group. Optional. Branch: Assign the patient to a Branch. Branches are set up in the same location as Units (File>File Maintenance>Entity>Type =Unit). Optional. Discharge tab Fields enabled after entering a Discharge Date for the patient. This information will print on the Discharge Summary.
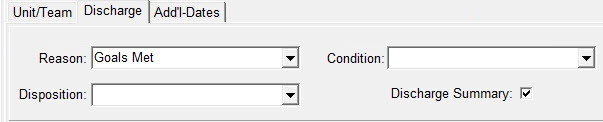
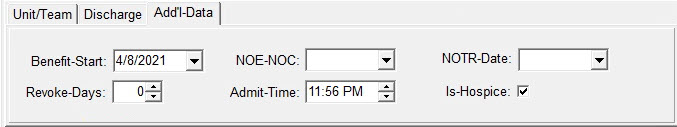
Reason: Enter reason for patient's discharge. Discharge Reasons can flow to Patient Status Code claim output to override the standard "01" Discharged status. Reason codes are set up under File>File Maintenance>Category>Type = Discharge Reason. Required when discharging a patient. Disposition: Enter disposition reason. Discharge Disposition can flow to Patient Status Code claim output to override the standard "01" Discharged status. Reason codes are set up under File>File Maintenance>Category>Type = Discharge Reason. Optional. Condition: Enter discharge condition. Optional. Discharge Summary: Defaults to checked. Flags the patient for "Discharge Summary" printing when selecting the option to print summaries for "All Flagged Patients" under Patient>Discharge Summary>General Options>Selection Type. You can also print the individual patient's discharge summary when highlighting the discharged admit record and clicking the "Print" button in Patient>Admit tab. Add'l Data tab Benefit Start: Enter the date the patient elected Medicare Hospice benefit. This information will populate from your clinical software if interfaced. This date is used to determine when Late Routine days begin. NOE/NOC Date: (Hospice patient) This date will be automatically populated if the NOE is marked submitted/printed via the Billing menu. The user can also manually enter the date Medicare accepted the patient's Hospice NOE. For Home Health patients, the NOA Date is shown instead. NOA/Date: (Home Health patient) This date will be automatically populated if the NOA is marked submitted/printed via the Billing menu. The user can also manually enter the date Medicare accepted the patient's Home Health Notice of Admission.For Hospice patients, the NOE/NOTR Date is shown instead. NOTR Date: This date will be automatically populated if the NOTR is marked submitted/printed via the Billing menu. The user can also manually enter the date the patient terminated or revoked hospice care. Revoke Days: Enter only for patients who revoked and reelected the hospice benefit within 60 days (otherwise leave blank). Enter the number of benefit days used. Determines when the patient Late Routine day begins (61st day of the benefit period). Admit-Time: enter the patient's admission time if needed for claim output (i.e. Palliative billing). Option set must be configured to pull Admit Date/Time. Is Hospice: This flag is posted from Clinical to indicate if the patient is admitted under a Hospice or Home Health Unit/Agency. For Home Health patients, the NOA Date field is shown to indicate the date an NOA is submitted electronically starting in 2022. For Hospice patients, the Benefit Start, Revoke Days, NOE/NOC, and NOTR Date fields are shown. |
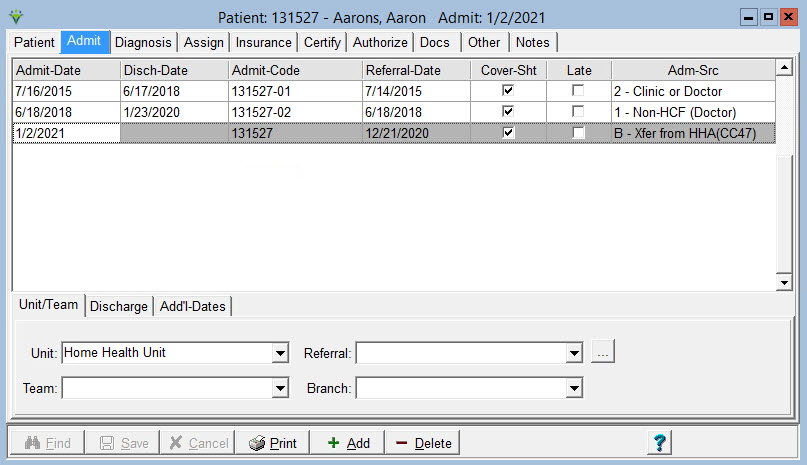
 button to add the record. For a referral patient, leave
the Admit-Date blank and enter only the Referral-Date.
button to add the record. For a referral patient, leave
the Admit-Date blank and enter only the Referral-Date.