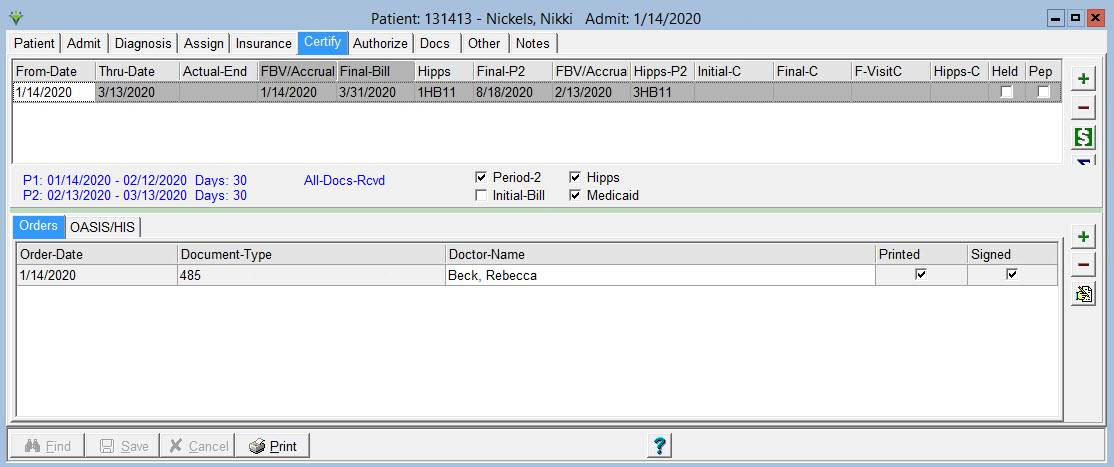
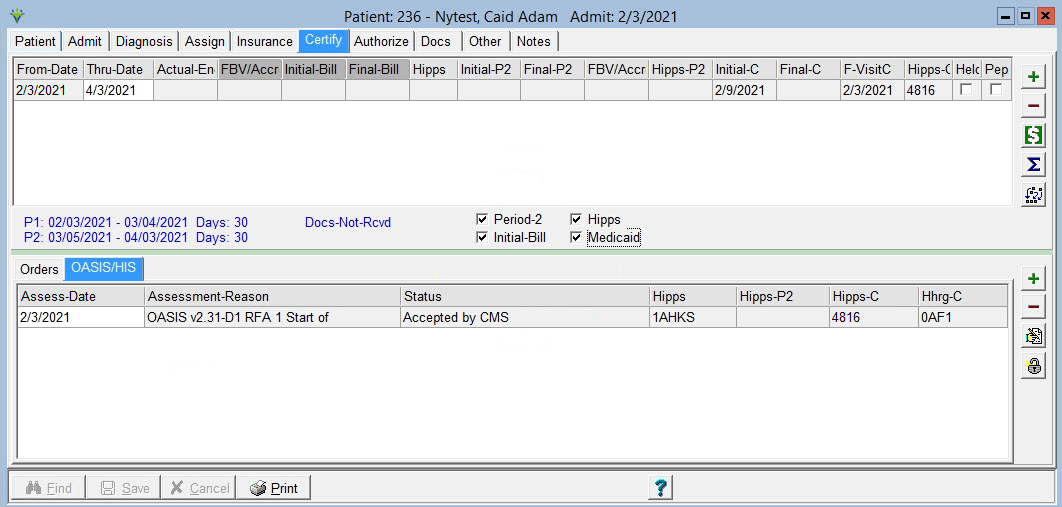
Click on PATIENT>ADMIT/MAINTAIN>Certify Tab
To Add a certification period on the Certify tab:
Press
the  button
to add the row.
button
to add the row.
From-Date: For the first certification period the From-Date defaults to the patient's admit date.
Thru-Date: Defaults to 60 days cert period but can be changed by the user.
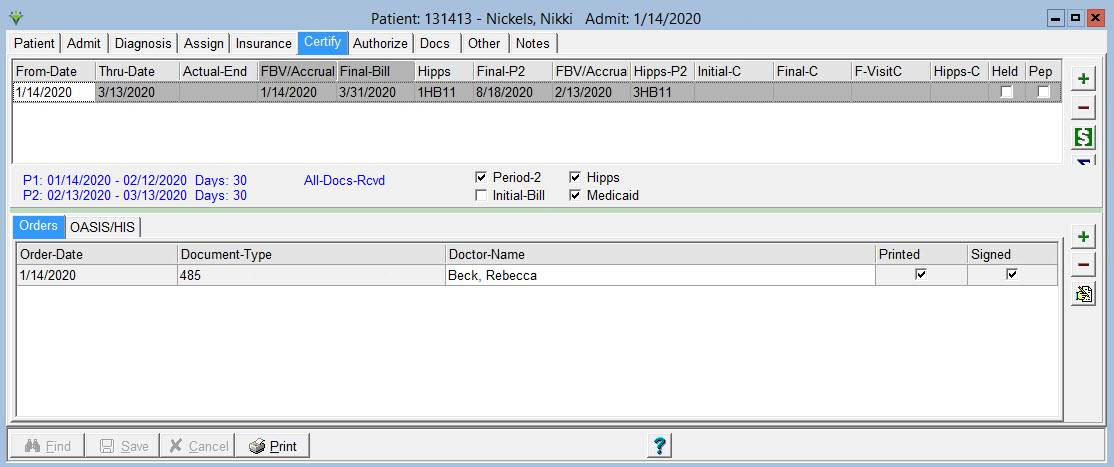
 : Click
this button to confirm dates for a 60 day or 90 day cert period (it will also calculate a 6 month cert if
option to allow cert dates greater than 90 days is selected in System
Settings>Data tab):
: Click
this button to confirm dates for a 60 day or 90 day cert period (it will also calculate a 6 month cert if
option to allow cert dates greater than 90 days is selected in System
Settings>Data tab):
Actual-End Date: This date will be filled in the the program when an Oasis Discharge Assessment is saved.
FBV/Accrual: For 2022 Finals-Only billing periods, this is the accrual date that is updated by the system once all information required is present and is used for PPS Revenue Reporting. An accrual date cannot be removed once generated to ensure the integrity of the revenue reports across months. For other billing periods this field is the first billable visit date, is updated when posting a RAP billing audit, and is used for the 0023 Revenue Code line on the RAP and Final claims. If this date is incorrect and needs to be changed, the RAP would need to be un-billed from Payments, the correct charge date entered in Charge>Enter/Maintain, and the RAP billing audit re-posted.
Initial-Bill: This is the Bill Date assigned when the RAP bill audit for this cert's first 30-day PDGM billing period was posted. A/R reports and claim generation require entering the bill date as selection criteria.
Final-Bill: This is the Bill Date assigned when the Final Bill Audit for this cert's first 30-day PDGM billing period was posted. Final claim generation requires entering the bill date as selection criteria.
Hipps: shows the calculated PDGM HIPPS case-mix for Period 1 from when the Billing Pre-Audit is run.
Initial-P2: This is the Bill Date assigned when the RAP bill audit for this cert's second 30-day PDGM billing period was posted. A/R reports and claim generation require entering the bill date as selection criteria.
Final-P2: This is the Bill Date assigned when the Final Bill Audit for this cert's second 30-day PDGM billing period was posted. Final claim generation requires entering the bill date as selection criteria.
F-VisitP2: This is the first billable visit date for the cert's second 30-day billing period and updates when posting a RAP billing audit. If this date is incorrect and needs to be changed, the RAP would need to be un-billed from Payments, the correct charge date entered in Charge>Enter/Maintain or posted from clinical and the RAP billing audit re-posted.
Hipps-P2: shows the calculated PDGM HIPPS case-mix for Period 2 from when the Billing Pre-Audit is run.
Intial-C: This is the Bill Date assigned when the NY Medicaid EPS RAP bill audit was posted. A/R reports and claim generation require entering the bill date as selection criteria.
Final-C:This is the Bill Date assigned when the NY Medicaid EPS Final Bill Audit was posted. Final claim generation requires entering the bill date as selection criteria.
F-VisitC: This is the first billable visit date for the cert period.
Hipps-C: shows the HIPPS for NY Medicaid EPS.
Held: Check this box to mark a cert as Held. Billing staff can elect to not bill these records by excluding held certs from the Billing Audit run.
PEP: Check this box if a partial episodic payment adjustment applies (patient is discharged and re-admitted within 60 day episode or transferred in from another HHA)
All
Docs Rcvd: This box will become checked when all records on the
Patient>Docs tab have a Received Date present for documents dated
within the episode. Billing Audits can be selected to run for
only patients with All Docs Received. If interfacing with clinical
software this flag can be updated via sent and received dates exporting
to the Patient>Docs tab. Contact your clinical software vendor in
interested in this feature.
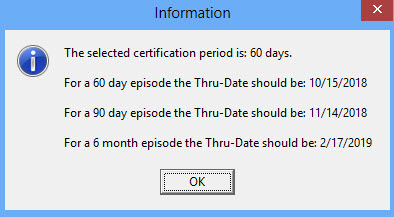
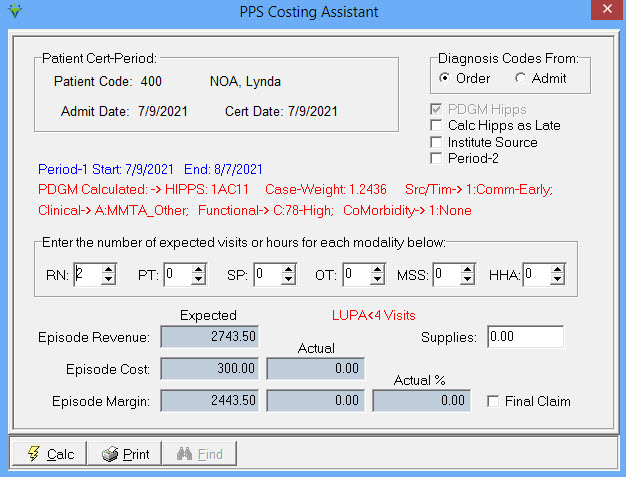
 : Click
this icon to use the PPS Costing Assistant and print the PPS Costing
Report. This utility calculates PPS or PDGM amounts based
on episode or period dates (it's not dependent on the insurance
PDGM Effective date). For Expected Episode Cost to calculate, average
cost $
must be assigned
to the modalities in the File>File Maintenance>System
Settings>Modality tab. If a Cost is assigned at the File > File
Maintnenance > Charge Code level, that cost amount will be used for
the charge, otherwise the System Settings modality amount will be
used. Check the 'Calc HIPPS as Late' to see what
the PEP calculation would be to compare against Medicare payment ('Calc
HIPPS as Early/Late' is grayed out for HIPPS starting with a '5' as
they are paid regardless of Early/Late timing.) Click the 'Calc' or
'Print' button to view the report. Episode Revenue is based on Quality
rates. If your agency doesn't submit Quality data, take 2% off the
amount shown.
: Click
this icon to use the PPS Costing Assistant and print the PPS Costing
Report. This utility calculates PPS or PDGM amounts based
on episode or period dates (it's not dependent on the insurance
PDGM Effective date). For Expected Episode Cost to calculate, average
cost $
must be assigned
to the modalities in the File>File Maintenance>System
Settings>Modality tab. If a Cost is assigned at the File > File
Maintnenance > Charge Code level, that cost amount will be used for
the charge, otherwise the System Settings modality amount will be
used. Check the 'Calc HIPPS as Late' to see what
the PEP calculation would be to compare against Medicare payment ('Calc
HIPPS as Early/Late' is grayed out for HIPPS starting with a '5' as
they are paid regardless of Early/Late timing.) Click the 'Calc' or
'Print' button to view the report. Episode Revenue is based on Quality
rates. If your agency doesn't submit Quality data, take 2% off the
amount shown.
Click on a certifcation period on the top half of the window, then click on Orders
or Assessment to add or view associated 485 and OASIS assessments or HIS records.
Check 'Medicaid' to view the NY Medicaid EPS rate instead of the Medicare HIPPS/HHRG scores for OASIS.
Back to Patient